By Barnaby de Hoedt
Cannabis has long been stigmatised as a ‘gateway drug’ to ‘harder substances’. This has always been a bogus claim. Studies have shown that, even among the heaviest cannabis users, the vast majority do not move onto opiates. Meanwhile, the relatively small number that have are most likely to have done so because the illegal status of cannabis has forced them into interacting with black market drug dealers who are pushing other unregulated drugs. Prohibition is the gateway to unsafe drug use.
And cannabis is now increasingly recognised as the opposite: “the exit drug”. That is, a way out of opioid dependence, and therefore the answer to the opioid crisis, which has hit epidemic levels in the US. Testimony and evidence alike show that cannabis is both a safe and effective alternative to opioids to treat chronic pain and a safe and effective detox drug for the alleviation of opioid withdrawal.
The Opioid Epidemic
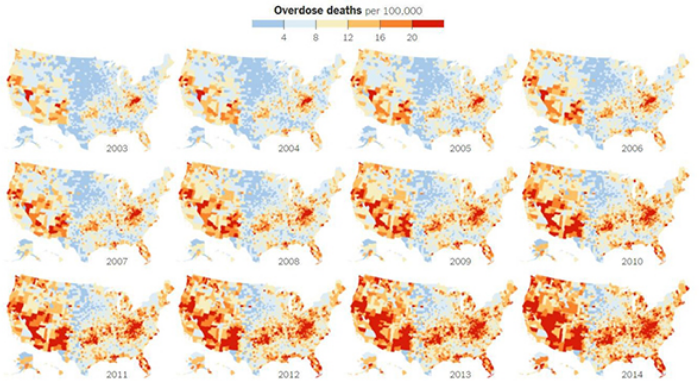
The roots of the current opioid crisis go back to around 1991 when Oxycodone emerged, marketed as a ‘miracle drug’ amid a national epidemic of chronic pain. US opioid prescriptions rose from 76 million in 1991 to 245 million in 2016.
Between 2000 and 2015, more than 500,000 people in the US – mostly poor working class people in neglected small towns and rural communities – died prematurely from both illegal and legal opioid drug use.
Legal prescription opioids kill more people than both heroin and cocaine combined. In 2016, more people (34,572) died after overdosing on prescription synthetic opioids such as fentanyl (20,145), or natural and semi-synthetic opioids such as oxycodone (14,427), than died from illegal heroin usage (15,446), cocaine (10,619) and methadone (3,314). (Source: US Centers for Disease Control and Prevention (CDC), September 2017.)
“Testimony and evidence alike show that cannabis is both a safe and effective alternative to opioids to treat chronic pain and a safe and effective detox drug for the alleviation of opioid withdrawal”
Opioids such as fentanyl are 50-150 times more potent than morphine, and have been criminally but legally prescribed for people who have no clinical need for such medication. Even those who have died from illegal opioid use such as heroin often first became addicted to legal synthetic prescription opioids.
The responsibility for this lies with pharmaceutical companies which manufactured the opioids, bribed doctors to prescribe them, and played down the risks. Hundreds of ‘sham’ speaking programmes and ‘educational’ events for doctors have been held at upscale restaurants. One New Jersey doctor received $136,768 from Insys Therapeutics. Insys spent $1.32m on speaking fees to doctors in 2016. In December 2016, several Insys executives and managers were arrested and charged with a nationwide conspiracy to bribe medical practitioners, many of whom operated pain clinics, to unnecessarily prescribe a fentanyl-based pain medication (Subsys) and defraud health care insurers.
Subsys is a potent and addictive narcotic intended to treat cancer patients suffering intense episodes of breakthrough pain. But in exchange for bribes and kickbacks, doctors wrote large numbers of prescriptions for patients most of whom were not cancer sufferers. Insys marketed the drug ‘off-label’ – ie for other types of pain for which it wasn’t approved. Furthermore, Insys targeted doctors they knew were not cancer doctors. More than 80% of Subsys scripts were off-label by 2015. One Insys salesperson’s motto for patients was to ‘start them high and hope they don’t die’. In 2016, 631,000 doctors received $2.8bn directly from ‘Big Pharma’ firms for meals, travel, consulting, speaking fees and so on.
Numerous US cities, counties and states have sued various makers of opioid painkillers for promoting the epidemic. Endo, Johnson & Johnson’s Janssen, Teva, Allergan and Purdue Pharma have all been named in an opioid marketing investigation by attorneys general from 39 US states. Major drug distributors in the US such as Mallinckrodt, Cardinal Health, AmerisourceBergen and McKesson have paid fines to avoid further legal action.
Mallinckrodt is one of the largest manufacturers of oxycodone, and in 2016 posted $3.4bn in revenue and a $489m profit. 500 million of Mallinckrodt’s oxycodone pills ended up in Florida between 2008 and 2012 – 66% of all oxycodone sold in the state. Yet the US government has taken no legal action against Mallinckrodt.
Instead, the company agreed to pay federal prosecutors a $35m fine and admit no wrongdoing. Mallinckrodt held that the Drug Enforcement Administration (DEA) has never required manufacturers to know their customers’ customers and that the agency provided the company with conflicting advice about its responsibilities under the law.

The DEA did not act to reduce the amount of narcotics the company was permitted to sell, nor provide guidance on how to track suspicious orders. For a company the size of Mallinckrodt, a $35m fine is a drop in the ocean. The DEA, Food and Drug Administration (FDA) and Federal Bureau of Investigation (FBI) have allowed the $13bn-a-year opioid industry to get away with misleading marketing and the aggressive, profit-pursuing distribution of opioids.
All these drugs – their manufacture, sale and addiction warnings – were approved by the FDA, a key defence cited by Big Pharma.
Although President Donald Trump declared the opioid epidemic a public health emergency in October 2017, he did not declare a national emergency, which would have released extra funding. The focus remains on punitive criminalisation of illegal drug usage, rather than on treatment of addiction. On 23 January 2018, a member of Trump’s Commission on Combating Drug Addiction and the Opioid Crisis, Patrick Kennedy, called the work of the commission a “sham” and a “charade”. The emergency declaration “has accomplished little because there’s no funding behind it”, he said.
Of the 11.5 million US citizens estimated to have misused prescription opioids, including 969,000 children aged 12-17, three million young adults aged 18-25, and the 2.6 million people diagnosed with opioid-use disorder (OUD) in 2015, only 1.1 million people received treatment. In 2015, opioid poisoning claimed the lives of 51 children under the age of five.
That’s the appalling human cost. In economic terms, the opioid epidemic is costing an estimated $504bn annually in health care expenditure, lost wages, sick days and criminal justice costs.
The Crisis In Britain
The opioid problem is growing here: in England, the number of patients admitted to hospital for overdosing on opioid painkillers doubled over the decade to 2016 to 11,660 people, and according to NHS Digital, the number of opioid prescriptions also doubled, to 24 million in 2016. Since December 2016, 88 deaths in Britain have been linked to fentanyl, which also killed the singer Prince. There are already 330,445 high-risk opioid users in the UK, the highest number in the EU, according to the Europe Drug Report.
A study published earlier in 2018 showed that in 2012, one in five people in Scotland received at least one opioid prescription, prompting the Scottish Government to commit to a review of national prescription policies for high-strength painkillers. The number of prescriptions of ‘strong’ opioids, including morphine, fentanyl, oxycodone and others, more than doubled from 474,385 in 2003 to 1,036,446 in 2012.
Ronnie Cowan MP of the Scottish National Party and the Green Party’s Caroline Lucas are both vocal campaigners for safe public injection facilities to be properly funded. Transform Foundation also backs what is called Heroin Assisted Treatement, which is legal in the UK but needs far more funding. It has proved to reduce infection rates, crime and health care costs.
The Entrance Drug
A person taking a relatively low dose of prescribed opioids is 15 times as likely to develop an opioid-use disorder (OUD) as a person who has not been prescribed any opioids. There is no safe level of semi-synthetic opioids. They should be removed from the market.
In the short Weedmaps documentary The Exit Drug, Mark Wallace, an anesthesiologist and Chair of the Division of Pain Medicine at University California San Diego, says: “A lot of heroin users got their start with opioid prescriptions.”
Many opioids are available in ultra-high dosages that exceed the CDC’s own safe limits. It says that “even relatively low dosages (20-50 morphine milligram equivalents (MME) per day) increase risk of overdose and death”.
It is important to state all this regarding the opioid crisis in an article about cannabis in order to show that cannabis is not ‘the gateway drug’. That opioid prescriptions have not been labelled as such until now is testimony to a bias motivated by vested interests.
Cannabis: Safe and Effective
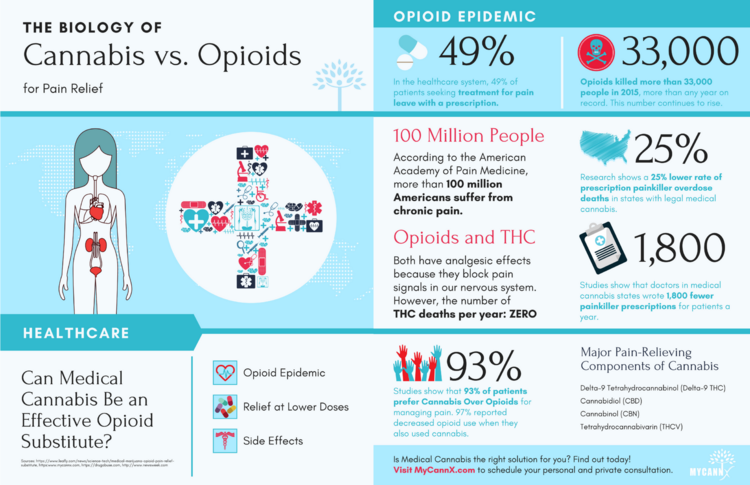
In 2016 the CDC published a set of guidelines aimed at curbing the opioid crisis, saying that a switch should be made to prescribing non-opioid drugs in cases of chronic pain.
Then, in June 2017, the National Academies of Sciences Engineering Medicine definitively concluded, from more than 10,000 studies in humans since 1999, that cannabis – not specific cannabinoids, not isolated cannabinoids, but that cannabis per se – is indeed safe and effective for the treatment of chronic pain. The CDC was asking for a non-opioid alternative and the National Academies gave them one – cannabis.
In the US states that have made medicinal cannabis legal, there has been an average 25% drop in fatal opioid overdoses. That effect gets larger as time goes on. For instance, in California, which has had a medicinal law since 1996, there is a 33% reduction in the opioid overdose rate.
Dr Adie Poe, a neuroscientist and clinical researcher at Washington University, St Louis, tells The Exit Drug documentary: “There is overwhelming, irrefutable evidence that cannabis is safe and effective. Cannabis is the gateway to getting out of opioid abuse. This is not my opinion, it’s the evidence. Cannabis is an effective and safe substitute for drugs like pain-relieving analgesics.
“The most exciting and promising value in medicinal cannabis is the sheer volume of people’s lives who will be improved. We’re not just talking about people who will stay alive because they didn’t stay alive on opioids; we’re also talking about all those people who are suffering and there is no alternative and no other drugs have worked.
“Cannabis probably has the greatest potential to have a major impact on public health specifically through its ability to diminish our reliance on opioids. This is cannabis’s greatest opportunity to do the most good in the world right now.”
Poe has studied the interaction between cannabis and opioids for more than 13 years. “The reason cannabis is an alternative to opioids is that is provides the same pain relief without the side effects,” she says. “When patients are given access to cannabis, they automatically reduce how much opioids they consume. If people are consuming fewer opioids then we have fewer opioid overdoses.”
Poe describes opioid withdrawal as “the seventh level of hell”. A person recovering from opioid addiction tells the documentary that “cannabis made the first few days much easier than any other detox programme I’ve been through. Cannabis really helps keep me off chemicals which would kill me.”
Joe Schrank, Programme Director of High Sobriety Treatment, backs this up: “As a social worker, one of our foundational principles is to reduce harm and to let people grow and determine their own life – cannabis allows us to do that. Cannabis makes the detox infinitely more tolerable.”
Roger Martin, founder of Grow for Vets, adds to the testimony. “91 people a day are dying of opioid prescriptions,” he says. “More than 50 veterans of the armed forces a day are lost to prescription overdose and suicide. We have thousands of veterans who have used cannabis to get completely off of opiates. We have tens of thousands more who have used it to dramatically reduce the amount of opiates that they take. Cannabis saved my life and it’s saved the lives of thousands of other people as well.”
Robert Milanes, ER physician and founder of Holistic on Call in California, tells the documentary that he started a medical marijuana practice because of the opioid epidemic. “People are not dying from overdoses of marijuana. There hasn’t been one case. Cannabis should not be the alternative, it should be the first line of treatment,” he says.

“It’s very hard to tell families that your child or family member died from opioids, and then go to the next patient complaining of pain and prescribe them the same thing that just killed this other person. I might as well say, ‘here’s a needle, here’s a syringe, you might as well just start heroin because this is where it’s going to end up’.
“I’ve been an ER physician for six years and I’ve been involved with medical marijuana for longer than a year. I’ve seen people die from heroin, I’ve seen kids die from taking opioids, I’ve seen people die from Benzo overdose – I have never seen someone die from marijuana.
“It is very tempting to tell patients that narcotics are not the answer, I think you should try medical marijuana, but the fact that it is federally illegal means providers are not doing it.”
Despite all the evidence and progress at state level, the FDA has told the DEA that cannabis remains unsafe.
“We know the abuse potential is low, and we know there are a lot of medicinal benefits,” says Wallace, but the federal authorities aren’t listening.
Restricted Research
“This is the catch 22 in medical cannabis research,” says Poe. “You can’t get data because cannabis is a schedule 1 [no medicinal value, high risk of abuse], and it stays schedule 1 because we can’t get enough data.”
The exact same problem exists in Britain, of course, only the situation is worse here because cannabis is illegal everywhere.
“I am a pharmacologist, and when I look at the cannabis plant, I see incredibly complex pharmacology,” says Poe. “I see hundreds of biologically active molecules which have a variety of effects on the brain and the body. In the FDA-approval process, typically their formula is that the drug is one molecule, and that there is one indication, one illness. If you think about the clinical use of cannabis medicine, it is neither of those things. It is not one molecule, it is not a standard preparation. It’s not just being used for pain, it is being used for anxiety, for PTSD, for insomnia, for Crohn’s, for many, many things. On both sides of the equation cannabis does not fit into the regulatory framework which the FDA has set up in order to bring an experimental drug, a pre-clinical drug into the marketplace.
“Cannabis probably has the greatest potential to have a major impact on public health specifically through its ability to diminish our reliance on opioids. This is cannabis’s greatest opportunity to do the most good in the world right now” – Dr Adie Poe, Washington University, St Louis
“The reason cannabis is an alternative to opioids is that it provides the same pain relief without the side effects.
“We discovered that the active molecule in the cannabis plant was delta-9-tetrahydrocannibinol in the 1960s but it wasn’t until the early 1990s that we identified what it was inside of our own bodies which activates the same receptors as THCs.”
Wallace continues: “We have cannabinoid receptors all over our bodies. They are located on inflammatory cells, white blood cells, lymphocytes, they are located throughout the nervous system. They have anti-inflammatory effects and various properties that have health benefits. When you stimulate the cannabinoid [type] 1 receptor you reduce pain transmission into the nervous system.”
Conclusion
Earlier in November, US doctor Frank D’Ambrosio told the World Health Organisation that he had stopped prescribing opioids to more than 10,000 patients in LA in the past five years and began prescribing cannabis instead. He said he was amazed at the results, and so he now campaigns across the world for better access to cannabis for everyone.
Dr Uma Dhanabalan in Dedham, Massachusetts is another doctor who says she has helped “thousands” of people by prescribing cannabis instead of opioids. Disdainful of politicians and doctors who “know jackshit” about cannabis, she sums it all up very nicely: “Cannabis is food, fuel, fibre, paper and medicine. We’ve replaced it [with] synthetic, synthetic, synthetic, synthetic, synthetic, synthetic. We’ve created illnesses because our bodies were not meant to be exposed to synthetics.”
The evidence is clear: prohibition mixed with opioids and the vested interests that boost them are the criminal entrance point to an appalling epidemic of hard drugs, addiction, illness and death. But finally the truth about cannabis – the exit drug – can no longer be denied.